COVID-19 Testing At Skilled Nursing Facilities: Guidance Based on PA DOH Advice
Responses to the COVID-19 pandemic have led to rapidly evolving recommendations, guidelines, and advice throughout health care. A recent publication from the Pennsylvania Department of Health’s Health Alert Network provides wide-ranging, general counsel for skilled nursing facilities (SNFs).
Testing Is Covered by Medicare
CMS has issued the necessary waivers and rule changes to enable Medicare Part B (the medical insurance component) to pay for testing for COVID-19 without a physician’s order.
Testing Should Be in Addition to Existing Interventions for Infection Prevention and Control (IPC)
Preliminarily, facilities will want to vigorously maintain their existing practices to prevent COVID-19 transmission, including such steps as:
- prohibiting all visitors except those essential to the delivery of essential services;
- prohibiting the pre-COVID-19 usual gatherings of residents/patients for exercise, rehabilitation, meals, U.S. mail, and other activities;
- temperature and symptom screening for all entrants into the facility;
- increased cleaning and sanitizing services throughout the facility;
- segregation of COVID-19 positive residents into zones, as explained below; and
- subject to the availability of qualified staff, and as detailed below, separation of symptomatic or COVID-19 positive employees and staff.
Who to Test?
Because COVID-19 can be insidiously transmitted by infected, yet asymptomatic people, ideally, there would be sufficient testing for facilities to test all residents and staff for an initial snapshot to help the facility tailor its practices, and then repeatedly until there are no positives. Absent universal testing, however, testing shortages may require prioritizing:
- facilities with no known cases among residents or staff may want to test a representative sample population (the Advisory suggests 20% of the residents and staff on a weekly basis);
- facilities with any known cases among residents or staff will want to test:
- all symptomatic residents and staff;
- asymptomatic, high-risk residents such as:
- spouses/partners/roommates of symptomatic residents and staff;
- residents returning from a hospital;
- direct admissions upon discharge from hospitals;
- residents whose medical needs require them to leave the facility (e.g., dialysis patients);
- staff who work at other long-term care facilities; and
- formerly-infected residents and staff who evidence appropriate indications of recovery.
Testing Documentation
The Pennsylvania Department of Health suggests documenting the patient’s agreement (or perhaps that of the patient’s medical power-of-attorney) using the same process as used for other lab tests.
Retesting – Who and When?
Ideally, weekly retesting could be conducted until the results return no new cases. Until testing becomes suitably available, however, retesting may be prioritized:
- all symptomatic residents and staff;
- people for whom testing is inconclusive;
- all infected staff before returning to work (for staff)
- all infected residents before returning to their pre-infection location;
- Pennsylvania’s Department of Health offers addition advice for discontinuation of precautions for COVID-19 patients here.
- residents who regularly leave the facility for essential medical treatments (e.g., dialysis patients);
- staff who work at other long-term care facilities where there may be COVID-19 cases;
- CMS expects that its new requirement for SNFs to report the number of all suspected and confirmed COVID-19 infections among residents and staff will allow it to begin publishing the names of specific SNFs and the number of COVID‑19 cases (suspected and confirmed) and deaths on a CMS data site by the end of May 2020.
Testing Goals: Facilitate Prevention Practices
Test results may help a facility accomplish specific practices to prevent the spread of the virus:
- Allocate – Test results identify the SARS-CoV-2 burden throughout the facility, allowing reconsideration of space and staff utilization.
- Separate – Resident test results may reveal exposed residents to be separated from those without detectable SARS-CoV-2 infection.
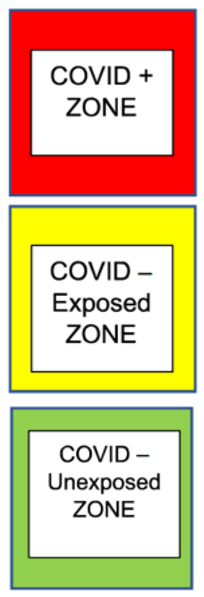
- Pennsylvania’s Department of Health suggests three resident-cohorts aimed at both quarantining infected residents and, to the extent that the available supply of qualified staff permits, segregating staff:
- “COVID +” (red zone) for residents who test positive.
- “COVID potential” (yellow zone) for symptomatic residents pending test results, for asymptomatic residents testing negative who are still within 14 days of possible exposure, for residents for whom testing was inconclusive, and for asymptomatic residents refusing to undergo testing for at least 14 days after exposure.
- “COVID unexposed” (green zone) for residents believed to have been unexposed to COVID-19.
- Ideally, facilities could segregate both staff and equipment within each zone. Facilities which need staff to work in more than one zone per shift will want to consult the Pennsylvania Department of Health’s specific guidance.
- Pennsylvania’s Department of Health suggests three resident-cohorts aimed at both quarantining infected residents and, to the extent that the available supply of qualified staff permits, segregating staff:
- Staff test results may reveal who should be entirely kept away from the facility.
- The Department’s guidelines acknowledge that when faced with a critical need for qualified staffing, a facility may need to engage asymptomatic yet nonetheless infected staff within the “red zone” for COVID + residents. In such circumstances, the Department asks facilities to ensure that such staff be limited to the “red zone,” and that the facility separate work areas, break rooms, work stations, and bathrooms for COVID + staff.
- Restore – Test results signal when it is reasonable (1) to allow excluded-staff to return to work and (2) to discontinue precautions for residents with resolved infections.
- For guidance regarding the return-to-work decision, you may find guidance from both White and Williams’ Return To Work Reference Guide and the Pennsylvania Department of Health’s Advisory 501.
As always, alerts from White and Williams are intended to provide general guidance. You will want to consult with White and Williams for specific counsel for your specific circumstances. If you have any questions please contact Bill Kennedy (kennedyw@whiteandwilliams.com; 215.864.6816) or another member of the Healthcare Group.
As we continue to monitor the novel coronavirus (COVID-19), White and Williams lawyers are working collaboratively to stay current on developments and counsel clients through the various legal and business issues that may arise across a variety of sectors. Read all of the updates here.
